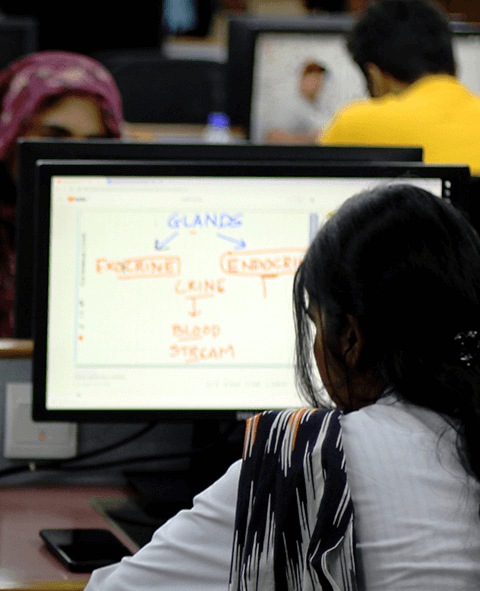
- Academics
-
Campuses
-
DMC
OJHA
-
Dow Institute of Medical Technology
Dow International Medical College
Institute of Bio Medical Sciences
National Institute of Diabetes & Endocrinology
Dow College of Pharmacy
Dow College of Biotechnology
Institute of Business and Health Management
Dow Institute of Nursing and Midwifery
Dow Institute of Radiology
School of Public Health
Institute of Behavioral Sciences
Dr. Ishrat-ul-Ebad Khan Institute of Oral Health Sciences
School of Dental Care Professionals
Dow Institute of Health Professional Education
Institute of Biological, Biochemical & Pharmaceutical Sciences
National Institute of Solid Organ & Tissue Transplantation
Dow Institute of Physical Medicine & Rehabilitation
School of Post Graduate Studies
Ojha Institute of Chest Diseases
Department of Clinical Haematology & Bone Marrow Transplantation
Dow University Hospital
Department of Pulmonology
Dr. Ishrat Ul Ebad Khan Institute of Blood Diseases
Dow Institute of Cardiology
National Institute of Liver & GI Diseases
Pharmacy Services
- Admissions
- ORIC
- Lab & Radiology
- Life at DUHS
- QEC
- Convocation 2023
- International Conference
- Dow Connect
- Staff Portal
- Student Portal
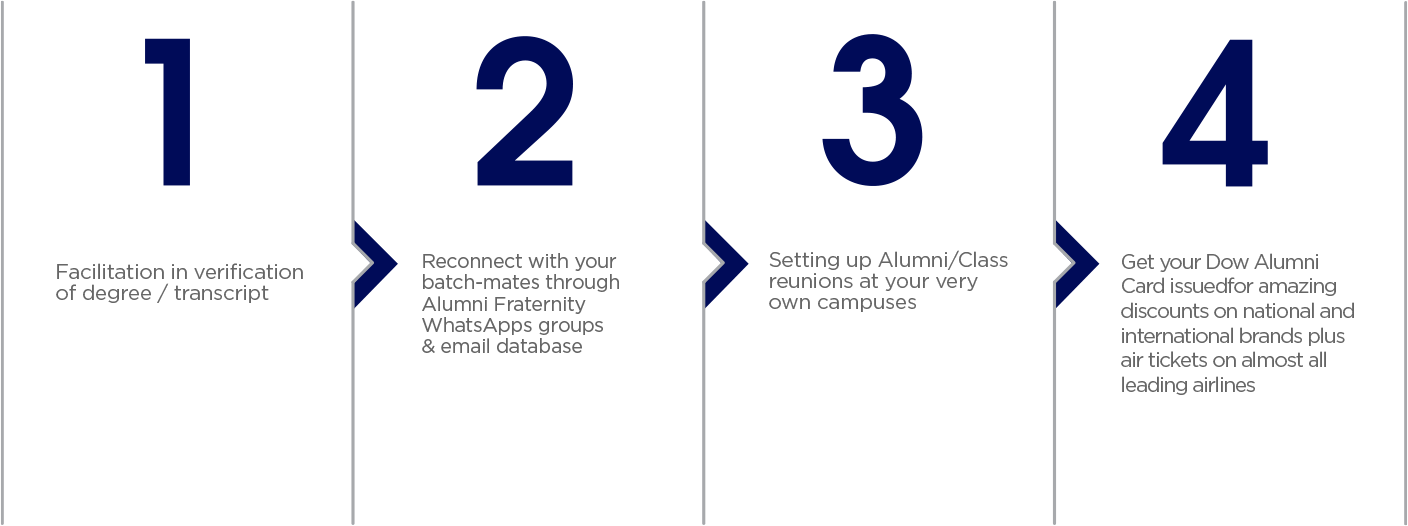
- Alumni Portal
- Donate Now!
Get in Touch
Baba-e-Urdu Road Karachi, Sindh, Pakistan